COVID-19 and nutritional management
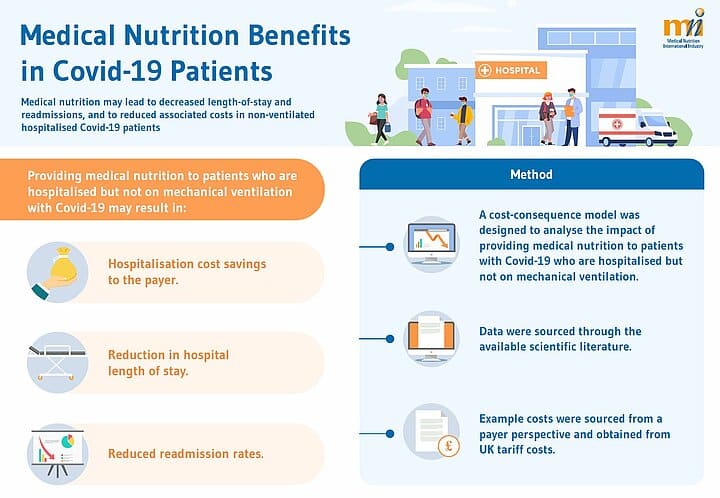
Medical Nutrition can provide benefits in Covid-19 patients.
Prevention, diagnosis and treatment of malnutrition should be routinely included in the management of COVID-19 patients. Medical nutrition may lead to decreased length-of-stay and readmissions, and to reduced associated costs in non-ventilated hospitalised Covid-19 patients
Resources
Factsheet: ''Medical Nutrition Benefits in Covid-19 Patients''
Based on the available evidence, MNI members have compiled data on the role of medical nutrition in non-ventilated hospitalised COVID-19 patients, it resulted in the following key findings:
- Reductions in hospital length of stay of approximately 12 days;
- Reduced readmission rates;
- Hospitalisation cost savings estimated to 6000 euros per patient.
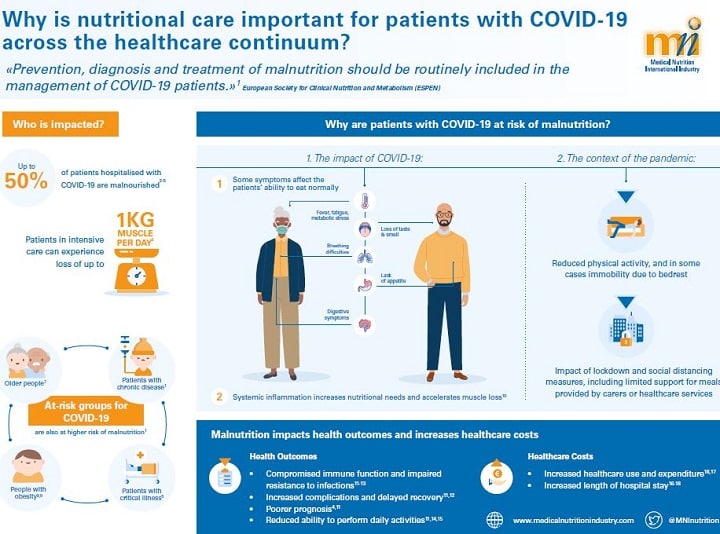
Infographic: "Why is nutritional care important for patients with COVID-19 across the healthcare continuum?"
Screening for malnutrition and timely nutritional intervention should be an integral component of care for patients with COVID-19 as malnutrition impacts health outcomes and increases healthcare costs. In this infographic, we provide recommendations for healthcare professionals, decision-makers and patients on why nutritional care is important for patients with COVID-19 across the healthcare continuum.
Guidance and Recommendations
ESPEN 10 recommendations “Nutritional management in individuals at risk for severe COVID-19, in subjects suffering of COVID-19, and in COVID-19 ICU patients requiring ventilation”
- Check for Malnutrition: Patients at risk for worst outcomes and higher mortality following infection with SARS-Cov-2, namely older adults and polymorbid individuals, should be checked using the MUST criteria or, for hospitilized patients, the NRS-2002 criteria.
- Optimisation of the nutritional status: Subjects with malnutrition should undergo diet counselling from experienced professionals.
- Supplementation with vitamins and minerals: Subjects with malnutrition should ensure supplementation with vitamin A, vitamin D and other micronutrients.
- Regular physical activity: Patients in quarantine should continue regular physical activity while taking precautions.
- Oral nutritional supplements (ONS): ONS should be used whenever possible to meet patient’s needs, when dietary counselling and food fortification are not sufficient to increased dietary intake and reach nutritional goals.
- Enteral nutrition (EN): In patients, whose nutritional requirements cannot be met orally, EN should be administered. Parenteral nutrition (PN) should be considered when EN is not indicated or insufficient.
- Medical nutrition in non-intubated ICU patients: If the energy target is not reached with an oral diet, ONS should be considered first and then EN treatment. If there are limitations for the enteral route, it could be advised to prescribe peripheral PN in the population not reaching energy-protein target by oral or enteral nutrition.
- Medical nutrition in intubated ICU patients I: EN should be started through a nasogastric tube; post-pyloric feeding should be performed in patients with gastric intolerance after pro kinetic treatment or in patients at high)risk for aspiration.
- Medical nutrition in intubated ICU patients II: In ICU patients who do not tolerate full dose EN during the first week in the ICU, initiating parenteral nutrition (PN) should be weighed on a case-by-case basis.
- Nutrition in ICU patients with dysphagia: Texture-adapted food can be considered after extubation. If swallowing is proven unsafe, EN should be administered.
Scientific articles
News
Opinions differ about whether Hippocrates really once said, “Let food be thy medicine and medicine be thy food…”, and what







