Nutritional care and cancer
Integrate nutritional care to maintain the quality of life of cancer patients.
Malnutrition in cancer patients leads to complications, poorer quality life, and increasing costs to healthcare systems.
Patients with cancer are more likely to develop malnutrition; level of risk is dependent on cancer type, stage or the patient’s age. It has been reported up to 70% of cancer patients can become malnourished.
Patients with gastrointestinal cancers, at more advanced cancer stages or older patients, are more likely to develop malnutrition due to the disease.
Malnutrition results in an increased burden to healthcare resources, with an estimated cost of €17 billion/year in the EU.
A recent World Health Organization (WHO) report notes that appropriate nutritional care helps cancer patients cope better with their illness and treatment.
Nutritional care should be an integral part of cancer care across Europe.
Cancer-related malnutrition affects patients and adds burden to healthcare systems, yet it is not sufficiently addressed. Cancer treatment typically targets cancerous cells and tumours, while cancer-related symptoms and complications are not routinely addressed and integrated in the care pathway, despite their significant impact on patients’ outcomes.

Resources
Oncology dossier
This document (as an evidence repository )is intended to provide all stakeholders with an up-to-date and practical summary of all available evidence based on cancer-related malnutrition and the clinical, economic and humanistic value of medical nutrition interventions, including oral nutritional supplements (ONS), enteral tube feeding (ETF), and parenteral nutrition (PN).


Cancer care: why nutrition matters
Malnutrition in cancer patients leads to poorer health outcomes. It also results in an increased burden to healthcare resources. Nutritional care should be an integral part of cancer care.
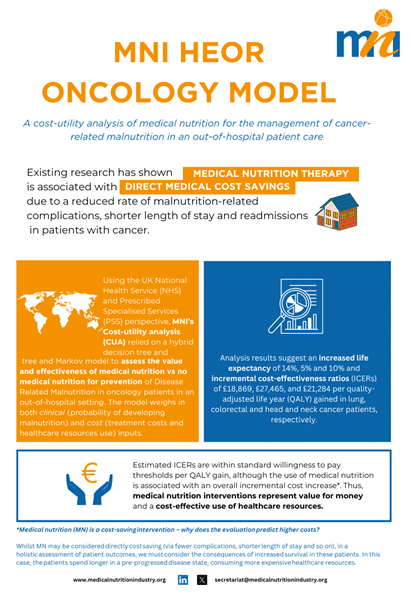
Cost utility of medical nutrition for the management of cancer-related malnutrition
MNI commissioned an independent impact assessment to evaluate the cost utility of medical nutrition for the management of cancer-related malnutrition in an out-of-hospital setting.
This analysis used the perspective of the UK National Health Service (NHS) and Prescribed Specialised Services (PSS) and utilised a hybrid decision-tree and Markov model to assess the cost-effectiveness of medical nutrition versus standard of care (no medical nutrition) on a hypothetical cohort of patients.
Videos
News
Opinions differ about whether Hippocrates really once said, “Let food be thy medicine and medicine be thy food…”, and what